Local hyperthermia
- Home
- Local hyperthermia
- Local Hyperthermia as a major tool in treating Cancer patients successfully in a non-toxic way
- Why are IQ scores declining over the previous 20 years?
- Expert report regarding the clinical use of CBD
- CBD effective in Healing Bone Fractures at all Ages and Prevention and Cure of Osteoporosis and Arthrosis
- Medical Cannabis Approval Sweeps Across Europe
- More people die from overdosing on pharmaceutical drugs than illegal drugs
- Flu vaccine BOMBSHELL: 630% more “aerosolized flu virus particles” emitted by people who received flu shots… flu vaccines actually SPREAD the flu
The local hyperthermia is used to selectively kill cancer cells. This therapy is applied specifically to the area of the tumor, referred to as local, localized, or regional hyperthermia. In MCC, local hyperthermia is used with all cancer patients who have solid tumors. It is an approach in which heat is only initiated in the tumor cell and leaves a healthy cell unaffected.
Local hyperthermia is exceptionally safe because it increases the temperature of cancer cells within the tumor to 42° C (107.6° F) without increasing the temperature of adjacent normal cells or in the rest of the body. Research has shown that cancer cells begin to die (necrosis) at 38.8° C (101.8° F) and at 42° C (107.6° F) almost all cancer cells are destroyed.
-
Local Hyperthemia Celsius TCS

Patient receiving local hyperthermia for liver cancer.
Cancer cells have an abnormal metabolism. Normal cells found throughout the body produce carbon dioxide as a waste product. In contrast, malignant cells produce lactic acid. When the cancer cells within a tumor are heated to 42 C (107.6 F), the production of lactic acid increases rapidly and the cells become highly acidic (pH goes down).
As metabolism speeds up within the tumor cells, they essentially self-destruct and drown in the lactic acid they produce. Healthy tissue surrounding the cancer cells are unaffected by the localized heat used in the treatment. The same biological dynamics occurs to a reduced degree during normal fevers 101.3° F (38.3° C) in which cancers become more and more under stress and produce more lactic acid
-
Making Cancer Visible to the Immune System
Cancer cells are also able to hide (cloak) from the immune system thereby avoiding detection. Fever-range, total-body hyperthermia and local hyperthermia both disrupt this cloaking mechanism. Whether is is local or total-body hyperthermia, each degree increase in temperature, causes cancer cells to undergo greater stress until the lactic acid production has increased to such a degree that the cancer cell is threatened with suffocation. The cancer cells will try to fight off their impending death by putting all their energy into surviving, thus dropping their escape mechanisms. Once a cancer cells drop their escape mechanisms, they are more easily detected by dendritic cells which now can better ”see” the “naked” or uncloaked cancer cells. As a result, the dendritic cells are better able to obtain an image of the cancer cells’ “ID”—its profile or antigen.
The electro-hyperthermia equipment used for localized hyperthermia causes no risk of burns and can be focused exclusively on any area of the body. Unlike total-body hyperthermia, with this localized technique we can selectively heat tumor cells.This enables us to provide interventions for areas of the body that would normally be difficult to treat such as the lungs, bone, and the head. The fact that hyperthermia can be efficacious in treating brain tumors was borne out by a recent Phase III study for patients with brain lesions, in which hyperthermia proved to support significantly better results in terms of illness-free time and survival when compared with radiation and/or medication.
Robert Gorter, MD, PhD, long term cancer survivor, founder and director, Medical Center Cologne
-
Safety and Effectiveness
Local hyperthermia is a highly effective means of destroying cancer cells without causing toxicity, particularly when used in conjunction with other immune supportive therapies such as vitamin C infusions, thymus peptides and mistletoe extract. In addition, most patients are provided with dendritic cell vaccinations since the heating process makes cancer cells more vulnerable for destruction by the immune system.
The efficacy of dendritic cell vaccinations is enhanced by simple injection them during or right after a fever period. At the Medical Center Cologne, even patients with primary or secondary brain tumors or metastases of the breast or lung, are successfully treated in this way without any side effects. Statistically, the research shows that about 72% of all patients withGlioblastoma multiforme Stage IV die within the first year after diagnosis only 1% survive for three years.
At the Medical Center Cologne, 48% of all patients with stage IV Glioblastoma multiforme go into complete and persistent remission, following a protocol of at least 3 dendritic cell vaccinations and 24 sessions of local hyperthermia.The electro-hyperthermia equipment used in this protocol was developed by the German company Celsius 42+.
-
Local Hyperthemia Research and Clinical Trials
As mentioned, approximately 2,800 articles have been published to date on “regional” or “local” hyperthermia. Among the 50 most recent studies on local hyperthermia, the majority (32 of the studies) involved the use of hyperthermia with chemotherapy. The majority of the other studies evaluated local hyperthermia in combination with surgery and with radiation. The others involved some form of immunotherapy provided in combination with the local hyperthermia treatments (primarily TNF-alpha—tumor necrosis factor-alpha).
Researchers have documented that conventional treatments such as chemotherapy and radiation, used in combination with local hyperthermia, clearly work more effectively with less side effects. Only a handful of large clinical trials have focused on local hyperthermia as a stand-alone treatment, perhaps due to the lack of economic incentives.
We predict that in the future, patients who desire a non-toxic approach to cancer will be treated with localized hyperthermia, paired with some form of immunotherapy such as those offered at the Medical Center Cologne.
-
References
Overgaard, J. (2006). Effect of hyperthermia on malignant cells in vivo: A review and a hypothesis. Cancer, 39(6), 2637-2646.
Patient's Experience at MCC
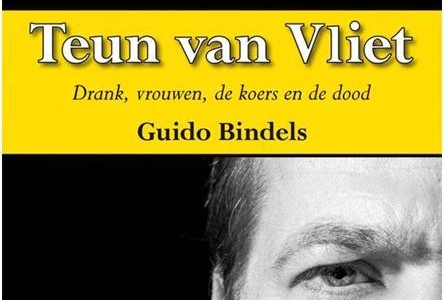
Twenty years ago, Teun van Vliet was twice an indoor world champion cyclist and in 1988 wore the yellow jersey in the Tour de France.
In 2001 he was diagnosed with a brain tumor and in 2006 an inoperable recurrence of the tumor was detected. Teun had another round of brain surgery (“debulking”) and also received radiation treatment. This caused him to lose his power of speech, and to some degree he also lost memory and coordination.Within conventional oncology, nothing could be done for him. He was told that he had a year left to live at the most. Teun and his girlfriend decided to seek a second opinion and they went to Cologne to consult with Dr. Gorter, who advised him to do local hyperthermia in combination with immune therapy.
Teun’s partner soon noticed beneficial changes in his health: “The first thing we noticed about these treatments was that they really improved his speech. He is much more lively; more active. I have my old buddy back, really. When he comes home from Cologne, his speech has improved, his motor skills have improved, he feels more energetic. Nothing but improvements. The quality of his life is definitely better. In April 2010, a new MRI scan confirmed that there is still no recurrence of the cancer and Teun has been clinically cancer-free for more than four-and-a-half years.
Teun van Vliet’s remarkable recovery from end-stage primary brain cancer has been written up in the following book: Bindels, G. (2010). Teun van Vliet-Drank, Vrouwen, de Koers en de Dood. Leeuwarden, The Netherlands: Elikser B.V.


 Deutsch
Deutsch Nederlands
Nederlands Turkish
Turkish Russian
Russian Italiano
Italiano Français
Français Português
Português العربية
العربية